Perfluorocarbon liquids (PFCL) have high specific gravity and optical clarity, which permit intraoperative retinal tissue manipulation. Perfluoro-n-octane (PFO; C8F18; Perfluoron, Alcon) has the most visible interface among other types of PFCL, which helps to have the best intraoperative removal rate.1 Generally, PFCLs have a postoperative subretinal retention rate of 0.9% to 11.1%, with a lower rate for PFO being in the 1% to 3.5% range.2,3 Risk factors for subretinal retention are large retinotomy of 120 degrees or more and failure to perform a saline rinse after fluid-air exchange.2
WHY REMOVAL IS VITAL
Pastor et al. showed that PFO has a toxic effect on the human retinal pigment epithelial (RPE) cells (ARPE-19).4 Elsing et al. also showed that histopathologic analysis of five eyes with retained PFO after vitreoretinal surgery for retinal detachment revealed an inflammatory response.5 This inflammatory response consisted mainly of macrophages with intracellular vacuoles containing PFO. However, removal of the PFO in all five eyes resulted in the resolution of the inflammatory response.5 Given the toxic effect of PFO on RPE and loss of retinal functions, subfoveal or sub-juxtafoveal PFO is often removed.6 However, sub-extramacular or subperipheral retina PFO does not result in a negative functional or anatomical outcome, and may be safely left alone2 (Figure 1).

REMOVAL TECHNIQUES
Direct aspiration. Several techniques have been described to remove the submacular PFO. One common approach is direct aspiration using a small gauge (36-gauge or smaller ) that is passed through the retina into the subfoveal space. The aspiration can be performed manually or via the extrusion line to enable foot pedal control.7-10 However, this method can damage the RPE and photoreceptors, and cause vision-threatening complications, such as choroidal neovascular membrane, macular hole, or submacular hemorrhage.11
Removal through slit. To minimize these risks, another method utilizes a 25-gauge microvitreoretinal (MVR) blade to create a small full-thickness slit above the PFO bubble, followed by the use of a soft-tip cannula to massage the subretinal PFO through the slit and displace it from the subretinal space.12
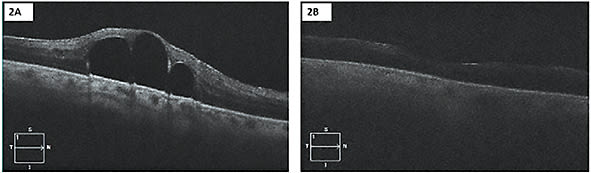
Transretinal aspiration. Another technique eliminates the need for any entry through the retina, but instead utilizes a 23- or 25-gauge silicone-tip cannula placed right above the retina overlying the subretinal PFO to aspirate the PFO transretinally with passive or active aspiration13 (Figure 2).
Displacement. Another technique that attempts to minimize the potential risks of direct aspiration of the PFO involves displacing the subfoveal PFO to a more peripheral location prior to removal. In this approach, a temporary therapeutic retinal detachment is created by injecting balanced saline solution into the subretinal space using a small-gauge cannula (36-gauge or smaller) in the peripheral macula.14 This detachment should involve the entire macula (or beyond) to allow the sub-foveal PFO droplet to move peripherally.
A few different methods can be utilized to manage the PFO droplet once it has moved away from the subfoveal location. One technique is to remove the displaced subretinal PFO using direct aspiration through the retina using a small-gauge cannula (36-gauge or smaller). Another technique is to make a small retinotomy just outside the macula through which to aspirate the subretinal PFO and balanced salt solution (BSS). Displacement of the PFO toward an inferior retinotomy may be aided by intraoperative patient head elevation and vibration.15
If the PFO has been displaced sufficiently peripherally, a technique of not removing the subretinal BSS and allowing the RPE to reabsorb the BSS has also been described in a patient—the subretinal PFO remained in a more peripheral location. One potential complication of this method is injecting the BSS at high pressure, which may rupture the thinned foveal neuroepithelium and create a full-thickness macular hole or cause RPE atrophy.14
Kim et al. described two cases of surgical removal of subfoveal PFCL through a subretinal BSS injection-induced macular hole, which subsequently closed with gas tamponade.16
CONCLUSION
Although surgical removal of retained submacular PFCL can improve vision and improve the secondary central scotoma, decreased vision or loss of retinal sensitivity does not necessarily indicate the need for surgery.17 Many patients with submacular PFCL have limited visual potential secondary to their retinal detachments, and the potential benefits and risks must be discussed with the patient.11,18 If the decision is made to remove centrally located submacular PFCL, the surgery is best performed within several weeks of detection to get the best potential visual outcome. NRP

REFERENCES
- Crafoord S, Larsson J, Hansson LJ, Carlsson JO, Stenkula S. The use of perfluorocarbon liquids in vitreoretinal surgery. Acta Ophthalmol Scand. 1995;73(5):442-445.
- Garcia-Valenzuela E, Ito Y, Abrams GW. Risk factors for retention of subretinal perfluorocarbon liquid in vitreoretinal surgery. Retina. 2004;24(5):746-752.
- Bourke RD, Simpson RN, Cooling RJ, Sparrow JR. The stability of perfluoro-n-octane during vitreoretinal procedures. Arch Ophthalmol. 1996;114(5):537-544.
- Pastor JC, Coco RM, Fernandez-Bueno I, et al. Acute retinal damage after using a toxic perfluoro-octane for vitreo-retinal surgery. Retina. 2017;37(6):1140-1151.
- Elsing SH, Fekrat S, Green WR, Chang S, Wajer SD, Haller JA. Clinicopathologic findings in eyes with retained perfluoro-n-octane liquid. Ophthalmology. 2001;108(1):45-48.
- Saatci AO, Koçak N. Retained submacular perfluorodecalin. Can J Ophthalmol. 2003;38(4):293-296.
- Lai JC, Postel EA, McCuen BW. Recovery of visual function after removal of chronic subfoveal perfluorocarbon liquid. Retina. 2003;23(6):868-870.
- García-Arumí J, Castillo P, López M, Boixadera A, Martínez-Castillo V, Pimentel L. Removal of retained subretinal perfluorocarbon liquid. Br J Ophthalmol. 2008;92(12):1693-1694.
- Roth DB, Sears JE, Lewis H. Removal of retained subfoveal perfluoro-n-octane liquid. Am J Ophthalmol. 2004;138(2):287-289.
- Joondeph BC. Controlled aspiration of subfoveal perfluorocarbon liquid using a novel microcannula. Retina. 2011;31(5):991-993.
- Lesnoni G, Rossi T, Gelso A. Subfoveal liquid perfluorocarbon. Retina. 2004;24(1):172-176.
- Charles S. Intricacies of the Use Of Perfluorocarbon Liquids. Retinal Physician. 2012;9(Oct):61-61.
- Erden B, Erdenöz S, Çakır A, Bölükbașı S, Elçioğlu M. Direct transretinal removal of subfoveal perfluorocarbon liquid combined with internal limiting membrane peeling. Ther Adv Ophthalmol. 2019;11:2515841419840244.
- Le Tien V, Pierre-Kahn V, Azan F, Renard G, Chauvaud D. Displacement of retained subfoveal perfluorocarbon liquid after vitreoretinal surgery. Arch Ophthalmol. 2008;126(1):98-101.
- Takahashi K, Kimura S, Hosokawa MM, et al. Release and extraction of retained subfoveal perfluorocarbon liquid facilitated by subretinal BSS, vibration, and gravity: a case report. BMC Ophthalmol. 2020;20(1):427.
- Kim JM, Woo SJ, Park KH, Chung H. Surgical removal of retained subfoveal perfluorocarbon liquid through a therapeutic macular hole with intravitreal PFCL injection and gas tamponade. Korean J Ophthalmol. 2013;27(5):392-395.
- Tewari A, Eliott D, Singh CN, Garcia-Valenzuela E, Ito Y, Abrams GW. Changes in retinal sensitivity from retained subretinal perfluorocarbon liquid. Retina. 2009;29(2):248-250.
- Suk KK, Flynn HW. Management options for submacular perfluorocarbon liquid. Ophthalmic Surg Lasers Imaging. 2011;42(4):284-291.








