Violence has no place in our society. Let’s start with that. According to the Centers for Disease Control (CDC), 20% of women report being victims of severe physical violence from an intimate partner.1
The coronavirus disease 2019 (COVID-19) started in China in late December of 2019 and has spread to the entire world, with approximately 4.5 million (and counting) deaths.2 In response to this, many governments adopted quarantines, social distancing, travel restrictions, and stay-at-home orders. Emerging data show that since the outbreak of COVID-19, reports of domestic abuse have increased both nationally and internationally.3,4 Many victims of abuse were forced to live with their abusers and had—and still have—limited access to supportive social resources.5
It’s not out of the realm of possibility that such abuse will present itself in your office. The following case report, for example, sheds light on how domestic violence can result in permanent vision loss. While the particular diagnosis in question is an important feature of this patient’s presentation, it is notable that the medical doctor has a fundamental duty to care for this patient in her entirety. Ophthalmologists and vitreoretinal surgeons are medical doctors first—and hold a responsibility to ensure that patients such as this are safe. Once such arguably more important elements are adequately addressed, the particular question in the retina is considered.
HISTORY AND CASE PRESENTATION
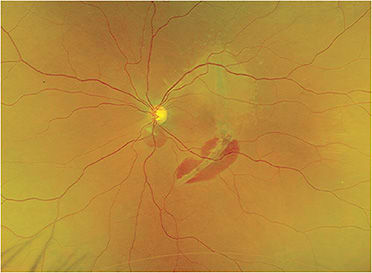
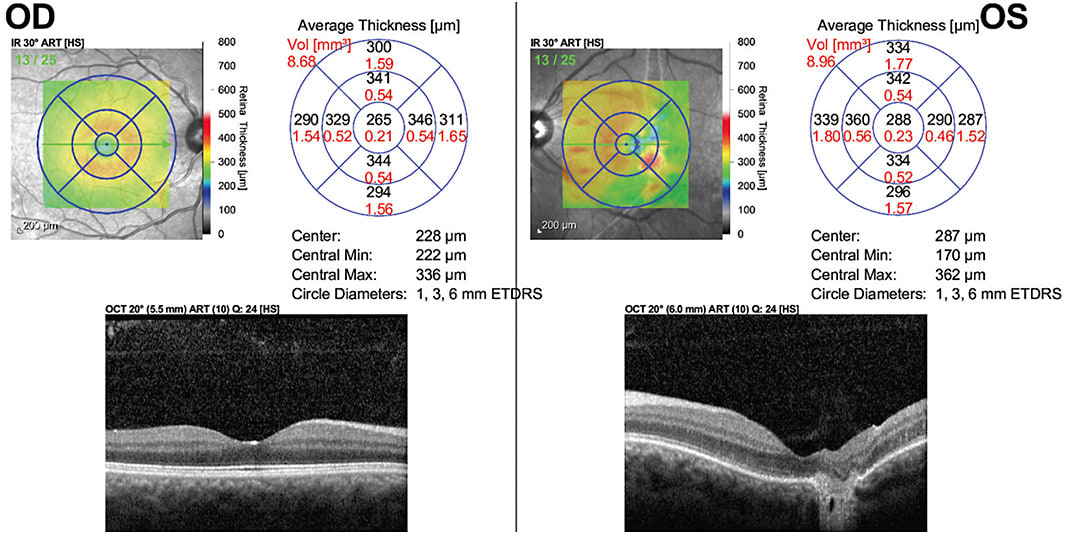
This patient is 38-year-old female who was recently a victim of domestic abuse. She noted decreased vision after fist-related facial trauma in the left eye. Her measured visual acuity was an eccentric 20/200. On dilated fundus exam, there was a white/yellow crescent-shaped subretinal lesion involving the fovea as well as subretinal blood both within the lesion and near the disc (Figure 1). Optical coherence tomography (OCT) showed disruption of the outer retinal layers, Bruch’s membrane, and retinal pigment epithelium (RPE) with extension into the choroidal layers in the right eye (Figure 2). Unfortunately, this patient has developed traumatic choroidal rupture.
DISCUSSION
Choroidal rupture was first described by Dr. Albrecht von Graefe in 1854. It involves a break in the choroid, Bruch’s membrane, and the RPE.
This diagnosis is made based on the history of a globe injury with a crescent-shaped white/yellow subretinal lesion concentric to the optic disc. Subretinal and sub-RPE hemorrhage can result at the time the choroidal rupture develops. This usually occurs secondary to blunt or penetrating ocular injury. Some have classified this finding as a result of direct or indirect accelerating compression/decompression. A direct choroidal rupture occurs anteriorly at the site of impact, generally parallel to the ora serrata and peripheral retina. In contrast, an indirect choroidal rupture occurs away from the site of impact, more posterior, and often concentric to the optic disc in a crescent shape.
An overwhelming majority (approximately 80%) of choroidal ruptures are indirect.6 Studies have found up to 5% to 10% of cases of blunt ocular trauma result in choroidal rupture.6 This includes sports injuries from projectiles, such as tennis balls, soccer balls, or hockey pucks,7 and even more diffuse injuries from air-bag deployment in motor vehicle accidents.8
The force buckles the globe in the area of impact and causes stress folding of the globe wall at a peripheral site, causing the choroid, RPE, and Bruch’s membrane complex to stretch and break. This can be more pronounced in those patients with brittle Bruch’s membranes, such as Ehlers-Danlos syndrome or angioid streaks, where minimal trauma can result in choroidal rupture.
The visual prognosis of these patients is based on the initial visual acuity and concurrent traumatic optic neuropathy. Of note, given the associated globe trauma, it is of paramount importance to rule out any orbital bone injury or retinal dialysis.
CONCLUSION
Given the imminent danger of residing within the home of her abuser, our patient has moved away from this region; therefore, there are no follow-up images to report. Since these patients are at high risk of choroidal neovascularization, she was given an Amsler grid and instructed to call should her vision change.
As retina specialists, we cannot forget our ethical duties as physicians and must always advocate for our patients, especially those patients in vulnerable situations. We pray that another similar case report is never reported again. Unfortunately, the likelihood of that would take a miracle. NRP
REFERENCES
- Centers for Disease Control and Prevention. What is intimate partner violence. Available at: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/fastfact.html . Last accessed Oct. 8, 2021.
- World Health Organization. Coronavirus disease (COVID-19) situation Report – 190. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200728-covid-19-sitrep-190.pdf?sfvrsn=fec17314_2 . Last accessed Oct. 8, 2021.
- Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38(12):2753-2755.
- United Nations UN News. UN chief calls for domestic violence ‘ceasefire’ amid ‘horrifying global surge.’ Available at: https://news.un.org/en/story/2020/04/1061052 . Last accessed Oct. 8, 2021.
- Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: increased vulnerability and reduced options for support. Int J Ment Health Nurs. 2020;May 7:10.
- Williams DF, Mieler WF, Williams GA. Posterior segment manifestations of ocular trauma. Retina. 1990;10 Suppl:S35-S44.
- Morris DS. Ocular blunt trauma: loss of sight from an ice hockey injury. Br J Sports Med. 2006;40(3):e5.
- Wang SH, Lim CC, Teng YT. Airbag-associated severe blunt eye injury causes choroidal rupture and retinal hemorrhage: a case report. Case Rep Ophthalmol. 2017;8(1):13-20.









